Research Article
Effect of Weight Loss on Markers of Inflammation and Endothelial Function in Childhood Obesity
Iezzi ML1*, Bruzzi P2, Lasorella S1, Predieri B2, di Pianella AV1 and Iughetti L21Paediatric Department, San Salvatore Hospital, University of L’Aquila, L’Aquila, Italy
2Department of Medical and Surgical Sciences of Mothers, Children and Adults, Pediatric Unit, University of Modena & Reggio Emilia, Modena, Italy
- *Corresponding Author:
- Maria Laura Iezzi
Paediatric Department, San Salvatore Hospital
University of L’Aquila, L’Aquila, Italy
Tel: + 3388544569
E-mail: marialaura.iezzi@libero.it
Received date: January 04, 2017; Accepted date: February 06, 2017; Published date: February 08, 2017
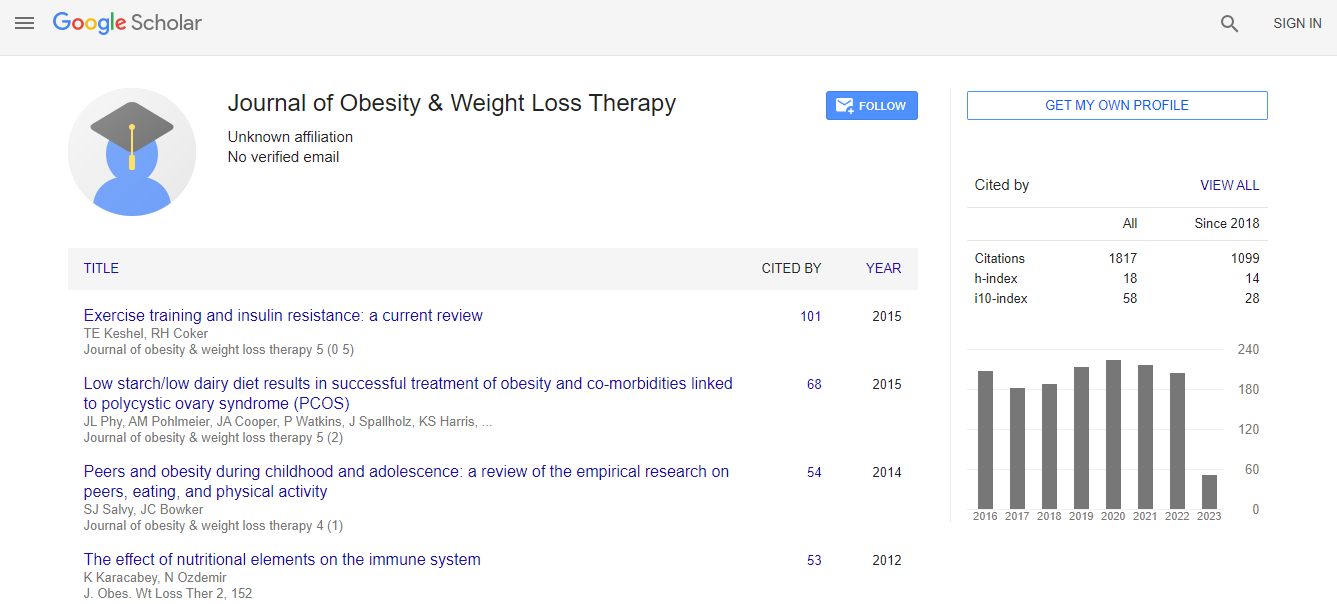
Citation: Iezzi ML, Bruzzi P, Lasorella S, Predieri B, di Pianella AV, et al. (2017) Effect of Weight Loss on Markers of Inflammation and Endothelial Function in Childhood Obesity. J Obes Weight Loss Ther 7:333. doi: 10.4172/2165-7904.1000333
Copyright: © 2017 Iezzi ML, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Obesity is associated with chronic low-grade and hyperinsulinism that may influence the progression of endothelial dysfunction and atherosclerosis already in childhood. Methods: To study changes in metabolic profile and markers of inflammation and endothelial activation in children with primary severe obesity after weight loss we involved 14 obese children (Ob) that underwent a lifestyle intervention and 18 normal weighted subjects (C). In Ob, anthropometric data were assessed both at baseline and after intervention together with oral glucose tolerance test and fasting evaluation of cholesterol assessment, interleukin-6, endogenous secretory receptor of advanced glycation end products and endothelin levels. Results: At baseline, serum IL-6 concentrations resulted significantly higher in Ob respect to C (12.96 ± 8.87 vs. 4.88 ± 1.19 pg/ml, p< 0.05). After weight loss, Ob significantly improved glucose metabolism and lipid assessment and they showed a significant reduction of all markers of inflammation and endothelial activation. In all subjects studied, BMI-SDS correlated positively with interleukin-6 (r 0.45, p < 0.05). Conclusion: Our results demonstrated higher concentrations of inflammatory markers in obese children compared to healthy subjects. Nevertheless, an early lifestyle intervention could improve the levels of these molecules together with cholesterol and glucose metabolism and may reverse the development of premature endothelial dysfunction in obese children.