Our Group organises 3000+ Global Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ 天美传媒 Access Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
天美传媒 Access Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
Citations : 2975
Indexed In
- Index Copernicus
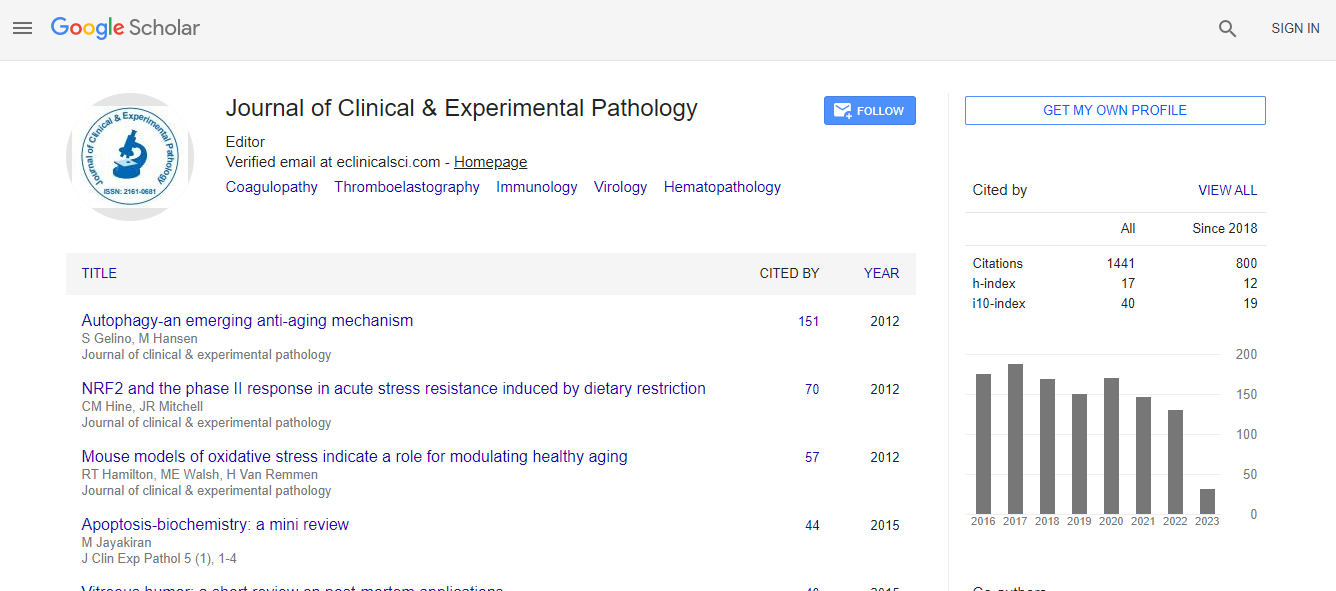
- Google Scholar
- Sherpa Romeo
- 天美传媒 J Gate
- Genamics JournalSeek
- JournalTOCs
- Cosmos IF
- Ulrich's Periodicals Directory
- RefSeek
- Directory of Research Journal Indexing (DRJI)
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- ICMJE
- world cat
- journal seek genamics
- j-gate
- esji (eurasian scientific journal index)
Useful Links
Recommended Journals
Related Subjects
Share This Page
Worse overall survival in breast carcinoma expressing p16
5th International Conference on Pathology
Gabriela Oprea-Ilies
Emory University School of Medicine, USA
ScientificTracks Abstracts: J Clin Exp Pathol
DOI:
Abstract
Genetic alterations affecting p16 protein is well described in human malignancies suggesting that inactivation of this pathway may be necessary for carcinogenesis. We aimed to study p16 in BC by immunohistochemical (IHC) methods in a large series of hormone receptor (HR) positive and triple negative tumors (TNT) in relation with demographic, pathologic features, biomarkers and clinical outcome. Invasive mammary carcinomas (IMC) diagnosed during a 7-year period were reviewed. The IMC markers ER, PR, and Her-2 scored by the new CAP standards were included. The tumors were studied as HER-2 positive, TNT, and hormone receptor (HR) positive. Tissue microarrays (TMAs) were stained with p16. P16 positivity was correlated with demographic and pathologic data and clinical outcome. Of the 157 IMC studied 37.6% where HR+ and 57.3% TNT. The age at diagnosis varied from 24-90 years. P16 was overall positive in 52.2%. Of the 75 p16 positive in AA, 12 were HR+ and 87%TNT vs. Caucasians who were 20% HR+ and 80% TNT. 85% of TNT showed statically significant p16 expression (p<.001) and they were correlated with basal-like BC, large tumor and high grade (all<.001). On univariate analysis, p16 positivity had a statically significant positive correlation with African-American (AA) race, TNT, large tumor size, high histologic grade and CK14 and it was inversely correlated with p53. Overall survival (OS) was statistically significant worse in p16 BC (p=0.0027), in the non-TNT (p=0.05) and in AA patients (p=0.001). In conclusion, p16 may constitute a prognostic marker and patients with p16 positive tumors may benefit from a more aggressive therapy. p16 expression may differentiate breast carcinoma subtypes and explain the more aggressive nature of TNT. High frequency of p16 positivity in breast cancers of African-American women may indicate different tumor biology.Biography
Gabriela Oprea-Ilies has completed her residency and fellowship in Pathology at the University of Minnesota and continued with a Cytopathology fellowship at Emory University Hospital, after which she remained on staff. She is the Director of the Immunohistochemistry Laboratory at Grady Memorial Hospital in Atlanta and the Medical Director of an independent Molecular Lab in Atlanta, Georgia. She has published more than 25 papers in reputed journals and serves as an Editorial Board Member and as reviewer of medical journals of repute.
Email: goprea@emory.edu